Conceptual model of ARDS
ARDS is an acute diffuse, inflammatory lung injury precipitated by a predisposing risk factor such as pneumonia, non-pulmonary infection, trauma, transfusion, burn, aspiration, or shock. The resulting injury leads to increased pulmonary vascular and epithelial permeability, lung edema, and gravity dependent atelectasis, all of which contribute to loss of aerated lung tissue. The clinical hallmarks are arterial hypoxemia and diffuse radiographic opacities associated with increased shunting, increased alveolar dead space, and decreased lung compliance. The clinical presentation is influenced by medical management (position, sedation, paralysis, and fluid balance). Histological findings vary and may include intra-alveolar edema, inflammation, hyaline membrane formation, and alveolar hemorrhage.
Diagnostic criteria
Criteria that apply to all ARDS categories
Risk factors and origin of edema
Precipitated by an acute predisposing risk factor such as pneumonia, non-pulmonary infection, trauma, transfusion, aspiration, or shock. Pulmonary edema is not exclusively or primarily attributable to cardiogenic pulmonary edema/fluid overload, and hypoxemia/gas exchange abnormalities are not primarily attributable to atelectasis. However, ARDS can be diagnosed in the presence of these conditions if a predisposing risk factor for ARDS is also present.
Timing
Acute onset or worsening of hypoxemic respiratory failure within 1 week of the estimated onset of the predisposing risk factor or new or worsening respiratory symptoms.
Chest Imaging
Bilateral opacities on chest radiograph and computed tomography, or bilateral B lines and/or consolidations by ultrasound, not fully explained by effusions, atelectasis, or nodules/masses.
Criteria that apply to specific ARDS categories
Non-intubated ARDS
PaO2/FIO2 ≤ 300 mmHg or
SpO2/FIO2 ≤ 315*
on
HFNO with a flow of ≥ 30 liters per minute or
NIV/CPAP with at least 5 cmH2O expiratory pressure.
Intubated ARDS
Mild: 200 < PaO2/FIO2 ≤ 300 or
235 < SpO2/FIO2 ≤ 315*.Moderate: 100 < PaO2/FIO2 ≤ 200 or
148 < SpO2/FIO2 ≤ 235*.Severe: PaO2/FIO2 ≤ 100 or
SpO2/FIO2 ≤ 148*.
Modified definition for resource-variable settings
SpO2/FIO2 ≤ 315*.
Neither positive end-expiratory pressure or a minimum flow rate of oxygen are required for diagnosis in resource-variable settings.
* - if SpO2 ≤ 97%.
Ultrasound operator should be well-trained in the use of ultrasound for identifying bilateral loss of lung aeration (e.g., multiple B lines and/or consolidations) and other ultrasound findings suggestive of non-cardiogenic pulmonary edema (e.g., pleural line abnormalities).
Modified oxygenation criteria can be applied in settings where arterial blood gas and/or HFNO, NIV, and mechanical ventilation are not routinely available.
Blood gas and oximetry measurements should be made when patient is comfortably at rest and at least 30 minutes after changes in position, FIO2, or flow rate. For pulse oximetry, ensure adequate waveform and oximeter placement. SpO2/FIO2 is not valid above saturation values of 97%. Pulse oximetry is not recommended for diagnosis if hemoglobin abnormality is suspected, e.g. methemoglobinemia
Illustrative cases
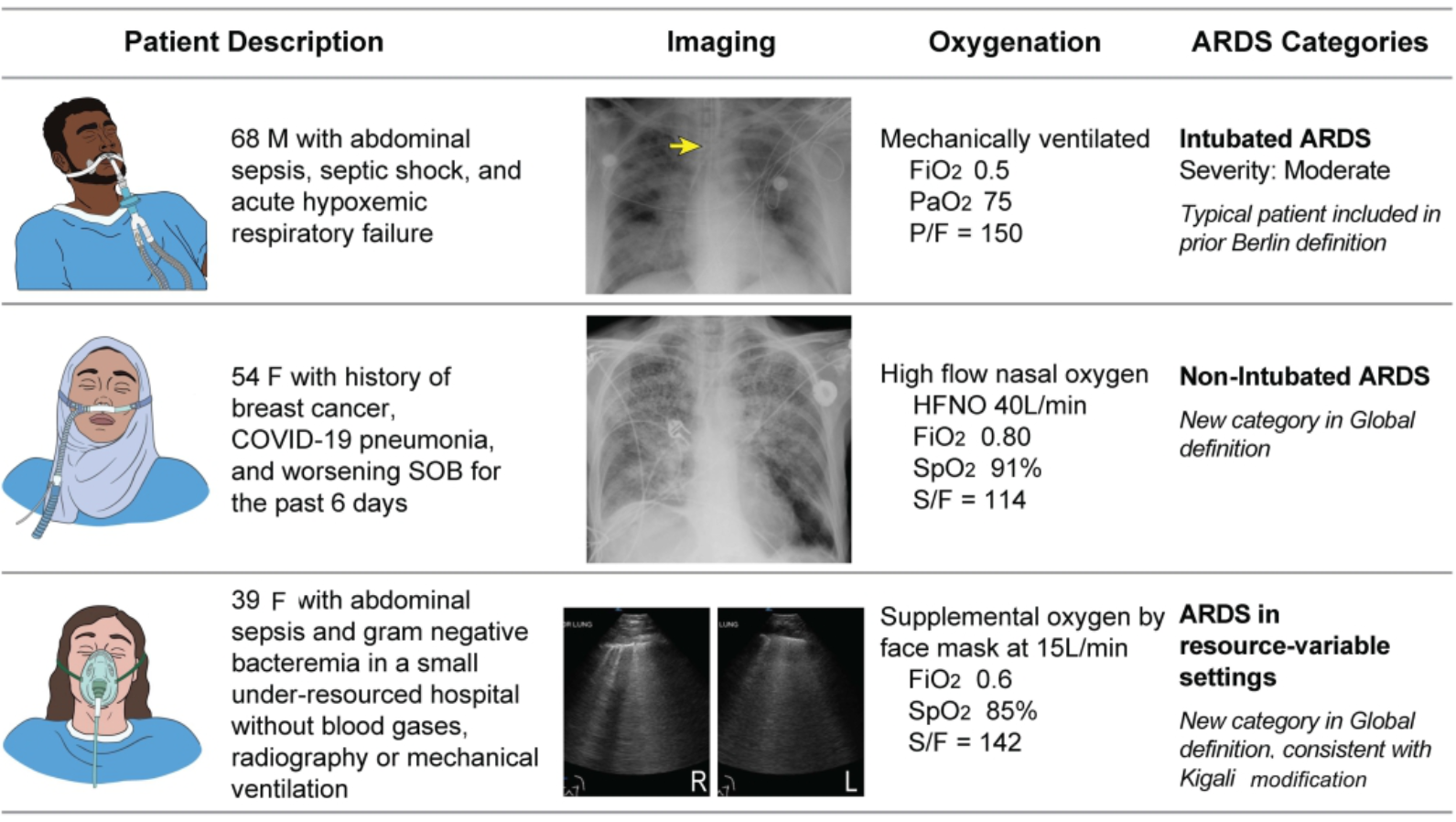
Illustrative cases with patient descriptions: representative lung imaging and oxygenation data for the three categories of ARDS in the Global Definition: intubated ARDS (top panel), non-intubated ARDS (middle panel) and ARDS in a resource-variable setting (bottom panel). Note the patient in the resource-variable setting can be identified with either an ultrasound (bottom panel, demonstrating bilateral diffuse Bline in non-dependent areas of the lung) or chest radiograph. Also, only the patient with intubated ARDS (top panel) meets criteria for the Berlin definition of ARDS. Arrow: endotracheal tube.
Am. J. Respir. Crit. Care Med. 2023. doi: 10.1164/rccm.202303-0558WS. Online ahead of print.